
 Some content associated with this program is only available via the Learn@ANZCA portal to registered users. To register for this program and learn more, check out the AEP page on the ANZCA website.
Some content associated with this program is only available via the Learn@ANZCA portal to registered users. To register for this program and learn more, check out the AEP page on the ANZCA website.
 Looking for education resources and information related to the Coronavirus/COVID-19 outbreak? Try the Coronavirus/COVID-19 guide.
Looking for education resources and information related to the Coronavirus/COVID-19 outbreak? Try the Coronavirus/COVID-19 guide.
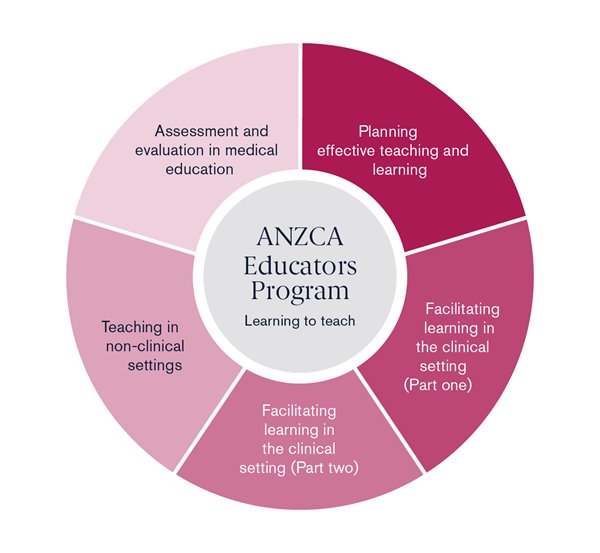
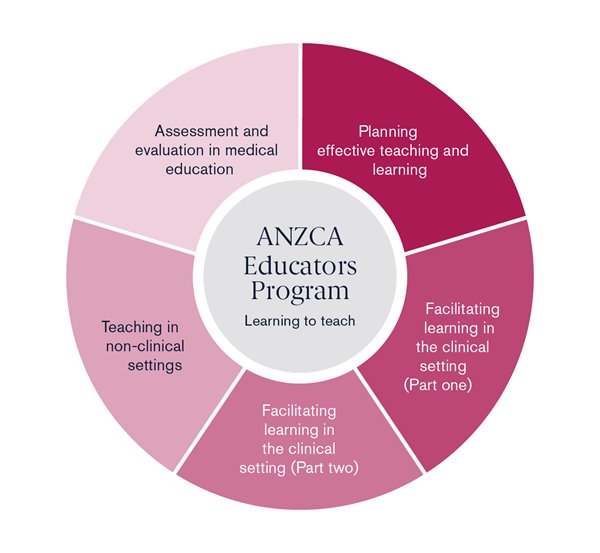
The ANZCA Educators Program (AEP) is a practical course designed to equip participants with the knowledge and skills to be competent clinical teachers. It is open to ANZCA fellows, specialist international medical graduates, provisional fellows and trainees (BT onwards), and to FPM fellows and trainees. A review of the AEP has been completed led by the ANZCA Educators Sub-Committee, with extensive input from AEP Facilitators and external experts. The Redesigned ANZCA Educators Program has been launched and now consists of:
Learning outcomes for the revised course are based on the progression indicators in Tier One (Knowing and Doing) of the recently-launched ANZCA Educator Competency Framework. This is the foundational level of competency, applicable to all ANZCA and FPM fellows in their role as clinical teachers.
The following Learning Outcomes underpin the content (interweaved throughout the modules):
Additionally, trainees are able to gain credits towards the “teach a skill” and “facilitate a group discussion/running a tutorial” activities (Scholar Role Activities).
Visit the AEP page on the ANZCA website for information on upcoming courses. If you are interested in becoming an AEP Facilitator, email us at aep@anzca.edu.au
**New learning outcome
*Significantly modified learning outcome
*Significantly modified learning outcome
*Significantly modified learning outcome
*Significantly modified learning outcome
**New learning outcome
**New learning outcome
 Can't find it? See our SOT support hub.
Can't find it? See our SOT support hub.
 Looking for the latest medical education resources? Check out our Medical Education guide.
Looking for the latest medical education resources? Check out our Medical Education guide.
Learn@ANZCA
Learn@ANZCA (formerly Networks) is the college's learning management system.
 Note: Some resources located in Learn@ANZCA require that you first register before accessing.
Note: Some resources located in Learn@ANZCA require that you first register before accessing.
Related courses


Quick links
About ANZCA
Copyright © Australian and New Zealand College of Anaesthetists.